Vaginal bleeding is a relatively common, but understandably distressing, occurrence for many women in the early stages of pregnancy (1,2). If you experience early pregnancy bleeding, it does not always mean that there is a problem or that something is wrong with your pregnancy (1-3). However, vaginal bleeding is sometimes a warning sign of more serious conditions, such as an ectopic pregnancy or miscarriage (1-4). Thus, all women who experience bleeding in early pregnancy must be promptly seen by a healthcare professional for a thorough assessment and diagnosis (1-3).
This post will explore the different causes of vaginal bleeding women experience in the first 24 weeks of pregnancy. We will also discuss when and how you should seek help and what commonly happens when women attend hospital for early pregnancy bleeding.

What are the causes of bleeding in early pregnancy?
(1) Implantation Bleeding
Implantation occurs when the fertilised egg (developing embryo) becomes embedded into the wall of your womb (2,3). This process can sometimes cause harmless light bleeding (or “spotting”) that usually presents around the time a woman’s period would have been due (2,3).
This type of bleeding is often pink or brownish in colour and should be very light (it should not soak through pads and/or underwear). Most women find that implantation bleeding only lasts for a few days, although it can occasionally last a little longer (3).
(2) Changes to the Cervix
Changes to the female hormones during the early stages of pregnancy can alter the cervix, increasing its blood supply and often making it softer. This can be known as an ‘ectropion’.
These pregnancy-associated cervical changes can make women more prone to bleeding after intercourse (known as “post-coital bleeding”). This sort of bleeding should be light and is harmless to you and your baby (3).
(3) Miscarriage
A miscarriage occurs when a pregnancy ends spontaneously before 24 weeks (3). Unfortunately, if you experience bleeding in early pregnancy, it can be a sign that you have had or are having a miscarriage (1-3, 5).
Miscarriages are common, with 1 in 5 women sadly having a miscarriage in the first 3 months of pregnancy without any identifiable cause (1,2).
Symptoms of miscarriage include (2,3,5):
🩺 Vaginal bleeding that might require a sanitary pad. This bleeding can vary from light spotting and/or a brownish discharge to heavy, bright red bleeding and/or blood clots.
🩺 Stomach pain, back pain and/or “cramping.”
🩺 Discharge of tissue from the vagina.
🩺 An end to traditional pregnancy-related symptoms that you might have been experiencing, such as nausea and breast tenderness.
The good news is that just because a woman has had a miscarriage, it does not mean that she is at any greater risk of having a miscarriage in future pregnancies.
In fact, most miscarriages are singular events and women have a good chance of having successful subsequent pregnancies (1). It is important to remember that a miscarriage is never your fault, and the majority of miscarriages could not have been prevented (2).
What is a threatened miscarriage?
Some women have a “threatened miscarriage,” which occurs when you experience the symptoms of a miscarriage (e.g. vaginal bleeding and/or pain) but an ultrasound scan demonstrates a pregnancy that is developing normally (1,3).
Luckily, many women who experience a threatened miscarriage are able to successfully carry their babies to term. Women in this situation might require a follow-up scan and/or additional appointment with a maternity care professional (e.g. in the early pregnancy assessment unit) (1).
If you would like more information on miscarriage (including recurrent miscarriage), we will be publishing a detailed blog post on this topic in the upcoming week.

(4) Subchorionic Hematoma
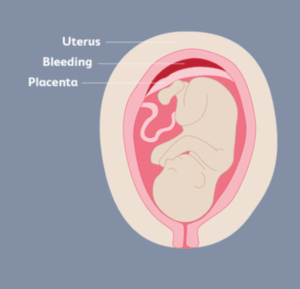
A subchorionic hematoma is a relatively common type of blood clot that develops when blood collects between the placenta and the wall of the uterus (6,7).
There is currently no clear cause for subchorionic hematomas, although experts believe that the following phenomena might play a role: the placenta becoming completely or partly separated from the uterine wall and/or an abnormal attachment of the developing embryo (fertilised egg) to the uterine wall during implantation.
Research has shown that women are more likely to develop subchorionic hematomas if:
- Conceived via assisted reproduction (e.g. IVF)
- They’ve already had at least one child
- They are older at the time of pregnancy (6).
Vaginal bleeding caused by a subchorionic hematoma can range from light spotting to heavy bleeding with clots (although it is also possible to have no bleeding at all) (6,7). Some women experience cramping alongside bleeding, especially if bleeding is on the heavier side (6).
What does a subchorionic hematoma mean for me and my baby?
A subchorionic hematoma should have no immediate or long-term impact on a mother’s health. The risk of pregnancy complications from a subchorionic hematoma depends largely on the size of the blood clot itself, the mother’s age and how far along she is in her pregnancy. In general: there is less risk associated with smaller subchorionic hematomas; those that do not grow as pregnancy progresses; hematomas that are present during the earlier stages of pregnancy (e.g. beginning of the first trimester) rather than those that develop later on; and those that are found on the surface of the placenta (rather than under the placenta or at the back of the fetal membranes) (6).
Research has shown that some subchorionic hematomas can increase a mother’s risk of a number of pregnancy complications, including miscarriage, placental abruption (where the placenta separates from the wall of the uterus before childbirth), pre-term labour (before the 37th week of pregnancy) and premature rupture of membranes (when your “waters break” before labour has begun) (6-8).
However, the majority of mother’s with subchorionic hematomas will have otherwise completely normal pregnancies and give birth to healthy babies (6).
Will I need any treatment for a subchorionic hematoma?
Once a subchorionic hematoma has developed, there is unfortunately no specific treatment for the blood clot.
Your maternity care team might recommend regular follow-up appointments to monitor the hematoma and baby’s well-being. You might also be advised to avoid physically demanding activities and strenuous exercise.
Importantly, most subchorionic hematomas would not require treatment even if such treatment existed (6).
(5) Molar Pregnancy
A molar pregnancy is an uncommon condition (affecting only 1 out of 700 pregnancies) where the placenta is abnormal and the baby is unable to develop normally (1, 9). There are two main kinds of molar pregnancy (9):
- Partial mole: A partial mole occurs when two sperm fertilise a normal egg. There might be some early signs of a growing fetus, but this will ultimately not develop into a baby.
- Complete mole: Complete moles usually occur when one sperm fertilises an abnormal “empty” egg that does not hold any of the mother’s genetic information. When this happens, a fetus cannot develop.
Unfortunately, neither partial or complete molar pregnancies can survive (9).
Symptoms of molar pregnancy include (9):
🩺 Vaginal bleeding or a dark coloured vaginal discharge (which might contain small lumps that resemble grapes). Bleeding and/or discharge most often occurs in the first trimester.
🩺 Extreme morning sickness.
🩺 An abnormally swollen stomach.
🩺 High blood pressure (this might be picked up by your GP or midwife).
🩺 Stomach pain.
🩺 Fatigue, weakness, nervousness, trembling and/or heat sensitivity (these are symptoms of an overactive thyroid gland).
What are the causes of a molar pregnancy?
The definitive cause of molar pregnancies is currently unclear, but there are some factors which have been shown to increase a woman’s risk of having a molar pregnancy. These include (9):
- Maternal age: specifically being a mother in her teenage years or over the age of 45.
- Previous molar pregnancy: for women who have previously had a molar pregnancy, the likelihood of having a second one is around 1 in 80; the chance of having further molar pregnancies among women who have had 2 or more is around 1 in 5.
- Ethnicity: women of Asian origin are around twice as likely to develop molar pregnancies as women from other ethnic backgrounds.
- Dietary Factors: low levels of carotene (a type of vitamin A) and folic acid have been linked with an increased risk of complete molar pregnancies. To ensure you and your baby are getting all the necessary vitamins, it is advisable to eat a healthy, balanced diet and take regular folic acid tablets for 2-3 months prior to pregnancy and for the first 12 weeks of your pregnancy. You should not take supplements that contain vitamin A, as too much can be harmful to your developing baby (a balanced diet should sufficiently meet this need).
What treatment will I need for a molar pregnancy?
As molar pregnancies are unable to survive, they will unfortunately have to be removed. This is usually done via surgical removal of the pregnancy (often via a process known as “suction removal”); it is a relatively straightforward procedure and most women are able to return home the same day (9).
Women in the UK who have had a molar pregnancy are registered with a specialist molar pregnancy centre to provide ongoing expert treatment and support. It is likely that your specialist centre will refer you for regular blood or urine tests at your local GP surgery for at least 6 months. These tests are done to check that your hCG hormone levels are returning to normal (these are often initially very high in women with molar pregnancies). Should you have any questions, concerns or complications following a molar pregnancy, your specialist team will be able to provide continued support and advice. (9)
Will a molar pregnancy affect my fertility?
A molar pregnancy should not impact your fertility and you have an excellent chance of having successful future pregnancies. As stated above, the chance of having a second molar pregnancy is small (approximately 1 in 80).
It is advisable to wait until you have completed all treatment for a molar pregnancy (this is around 6 months for most women) before trying to conceive again.
It is safest to use barrier contraceptive methods (e.g. condoms) until your hCG hormone levels have returned to normal; once these levels are normal, you are free to use any method of contraceptive that you wish (9).
A molar pregnancy can be a physically and emotionally draining experience for many women, and it can be helpful to discuss your feelings with someone you trust or others who have dealt with the same condition.
There is excellent support and friendly forums available to women who have suffered a molar pregnancy (run by women who have experienced one themselves) on: MyMolarPregnancy.com and Molar Pregnancy Support & Information.
(6) Ectopic Pregnancy
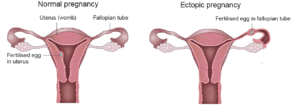
An ectopic pregnancy is one that develops outside of the womb (uterus), affecting around 1 in 90 pregnancies in the UK (3,10). In normal pregnancies, the fertilised egg travels from the fallopian tube to the uterus, where it then implants and the fetus begins to grow.
In an ectopic pregnancy, the fertilised egg implants and begins to develop outside of the uterus (most commonly in the fallopian tube, as seen from the image above). Sadly, ectopic pregnancies cannot survive and they can pose a significant danger to the mother. This is because, as an ectopic pregnancy develops and gets larger, it can burst (or “rupture”), damaging the mother’s anatomy and causing internal bleeding (10).
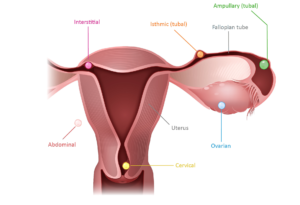
A much smaller group of women (around 3-5 out of every 100 ectopic pregnancies) are diagnosed with an ectopic pregnancy that has developed somewhere other than the fallopian tube. The image below shows some of the other locations where an ectopic pregnancy can occur (e.g. in the cervix or ovary) (10).
What causes an ectopic pregnancy?
Unfortunately, there is often no clear cause for an ectopic pregnancy and any woman of child-bearing age is potentially at risk. However, there are certain factors which are known to increase a woman’s risk of having an ectopic pregnancy, including (10):
- Having had a previous ectopic pregnancy
- Becoming pregnant while on the progesterone-only pill or a contraceptive intrauterine device (e.g. IUD or coil)
- A history of damage to the fallopian tubes (e.g. from previous infection of the fallopian tubes or surgery to the fallopian tubes)
- Being a smoker
- Conceiving via assisted reproduction methods (e.g. IVF)
However, it is important to remember that, even if one or more of these factors relate to you, it does not mean that you will have an ectopic pregnancy.
What are the symptoms of an ectopic pregnancy?
The symptoms of an ectopic pregnancy vary from woman to woman, and some women experience no symptoms at all. When women do experience symptoms, they commonly begin around the 6th week of pregnancy (10).
Symptoms of an ectopic pregnancy include (3, 10):
🩺 Vaginal bleeding that might be lighter, darker and/or heavier than your usual menstrual bleeding.
🩺 Lower stomach (abdominal) pain. This pain might come on suddenly, or it might come on more slowly over several hours or days. You might find that you only have pain on one side of your stomach.
🩺 Shoulder tip pain. Pain in the tip of you shoulder is caused by blood leaking from the site of the ectopic pregnancy into your abdomen and is unfortunately a sign that the condition is worsening. This pain is constant and not relieved by movement or painkillers. You might find that the pain is worse when you lie down.
❗You must seek urgent medical advice if you experience shoulder tip pain in early pregnancy (more information below).
🩺 Stomach upset. You might feel generally nauseous or have pain on opening your bladder and/or bowels. Some women also experience diarrhea.
🩺 Collapse, dizziness and/or severe stomach pain. If an ectopic pregnancy bursts (“ruptures”), you might feel sudden, excruciating stomach pain, dizziness and/or you might collapse. Very occasionally, a collapse is the first sign a woman has of an ectopic pregnancy.
❗Collapse, dizziness and/or severe stomach pain can be a sign of a life-threatening medical emergency. You must seek urgent medical attention (e.g. at your local Accident and Emergency department). There is more information on how and where to seek help below (10).
What is the treatment for an ectopic pregnancy?
Ectopic pregnancies cannot survive and, as such, the definitive treatment is to end the pregnancy. You and your maternity care professional will discuss the best treatment option for you, which is likely to depend on a range of factors, including: how far along you are in your pregnancy; your hCG blood hormone levels; your symptoms; and/or your fertility status (10).
There are usually three main treatment options available for women with an ectopic pregnancy (10):
(1) 👩⚕️ Expectant management (“wait and watch” approach)
Sometimes ectopic pregnancies self-terminate (end on their own), similar to a miscarriage. Some women are able to be treated with expectant management, which involves monitoring the hCG hormone levels with blood tests every few days to ensure that they return to normal.
Expectant management is usually only an option for women at the very early stages of an ectopic pregnancy who have minimal or no symptoms. Women in this situation should be given a contact number for the emergency gynecology services at their local hospital, should they have any concerns or develop worsening symptoms.
The success rate of expectant management varies largely from woman to woman, and you will likely need additional treatment (see below) if this approach fails to treat your ectopic pregnancy.
(2) 👩⚕️ Medical Management (Methotrexate)
Medical management involves an injection of a drug called Methotrexate which stops the ectopic pregnancy from growing, causing it to slowly disappear. Treatment with Methotrexate is most likely to be an option for women in the early stages of an ectopic pregnancy or with low blood levels of the hCG hormone.
Most women only require one dose of Methotrexate, although some (around 15% who undergo medical management), need to have a second injection to end their pregnancy. Unfortunately, approximately 7% of women who undergo medical management will still require surgery (see below) to successfully terminate their ectopic pregnancy.
Women who have medical management might need to stay in hospital overnight and will be required to have regular follow-up appointments to ensure their hCG levels are returning to normal. It is recommended that you wait at least 3 months before trying to conceive again if you are treated with Methotrexate.
(3) 👩⚕️ Surgical Management
Surgery for an ectopic pregnancy is performed under general anesthesia (while you are asleep) and will aim to completely remove the pregnancy. Depending on your personal situation, your surgery will either be:
- Laparoscopic (or “keyhole”): where surgery is performed via tiny cuts in your tummy (abdomen) with the help of a camera. Keyhole surgery is usually associated with a shorter stay in hospital and quicker recovery time.
- Laparotomy (or “open” surgery): this involves the surgeon making a larger cut into your tummy and likely means that you will need to stay in hospital longer after surgery and that your physical recovery will take more time (around 4-6 weeks for most women). Open surgery is used most often when the surgeon is concerned about significant internal bleeding from the pregnancy.
Most women will be advised to have their entire fallopian tube removed during surgery along with the ectopic pregnancy (this procedure is called a “salpingectomy“). The reason for this is that it gives you the best chance of being able to have a successful pregnancy in the future while reducing your risk of subsequent ectopic pregnancies (10).
However, women who only have one fallopian tube at the time of surgery or whose unaffected fallopian tube is damaged, might be advised to have a procedure known as a “salpingotomy.” In a salpingotomy, the surgeon will aim to remove the ectopic pregnancy but not the fallopian tube. Having a salpingotomy does unfortunately put you at a greater risk of subsequent ectopic pregnancies (due to damage sustained to the fallopian tube at the time of surgery), but it gives you a chance at having a future successful uterine pregnancy (10).
What if I present as an emergency?
When an ectopic pregnancy has burst or “ruptured”, women will require emergency life-saving surgery to control the bleeding. Emergency surgery will almost always involve removing both the ectopic pregnancy and the fallopian tube (salpingectomy). Depending on the situation and to act in your best interest, your surgeon might need to make the decision to operate quickly on your behalf (10).
Will an ectopic pregnancy impact my ability to conceive in the future?
For the majority of women, an ectopic pregnancy is a singular event and you have a good chance of having a successful pregnancy in the future. Reassuringly, the likelihood of conceiving a baby is only slightly reduced for women who only have one fallopian tube (10).
However, the risk of having subsequent ectopic pregnancies among women who have already had one is increased; around 7-10% of women who have had one ectopic pregnancy will have another, compared to just over 1% of the general UK population.
You should make contact with a healthcare professional (e.g. GP or midwife) early when you become aware that you are pregnant. Your maternity care team may offer you an earlier ultrasound scan to confirm that the pregnancy is growing in your uterus (10).
Getting help after an ectopic pregnancy
An ectopic pregnancy can be an extremely challenging, emotional and distressing situation for any woman. There can be a lot to process during and after treatment, including the loss of your pregnancy, impact on friends and family, affect on your future fertility and the dangers you may have experienced to your own health (10).
It is important to remember that you are never alone, and you should seek advice and support from a healthcare professional (such as your GP or a member of your maternity care team) if you are struggling (10). Some women may find it helpful to talk about their feelings with someone they trust, such as a partner, close friend or relative.
The Ectopic Pregnancy Trust offers extensive support to any woman impacted by an ectopic pregnancy. On their website you can find discussion forums, e-mail and Skype support, as well as contact information for their telephone helpline.
(7) Pregnancy of Unknown Location
Sometimes vaginal bleeding is the first symptom of a pregnancy of unknown location (PUL). A PUL means that you have tested positive on a pregnancy test but your pregnancy cannot be seen clearly on an ultrasound scan (1).
There are a few reasons why you might have a PUL, including (1):
- You are too early on in your pregnancy (or the pregnancy is too small) for it to be seen on an ultrasound scan. This can be the case even for normally progressing pregnancies in the womb, as they can not usually be visualised on a scan until around 3 weeks from conception (e.g. 5 weeks since your last period).
- You have had an early miscarriage. You might find that a pregnancy test remains positive up to two weeks after a miscarriage.
- You have an ectopic pregnancy that is currently too small to be seen on ultrasound.
Women who are told that they have a PUL will be followed-up regularly with the maternity care team to ensure that they receive an accurate diagnosis and appropriate support. Your follow-up care is likely to include a repeat ultrasound scan and regular monitoring of your hCG hormone levels with blood tests (1).
(8) Non-Pregnancy Related Bleeding
It is important to remember that, just because you are pregnant, it does not necessarily mean that vaginal bleeding has a pregnancy-related cause (4).
Other causes of vaginal bleeding include (4):
🩺 Bleeding from the urethra (e.g. from trauma)
🩺 Trauma to the cervix, vagina and/or vulva
🩺 Vaginal infections (e.g. thrush or sexually transmitted infections)
🩺 Cervical, vulva and/or vaginal cancers
🩺 Cervicitis (inflammation of the cervix)
🩺 Vaginitis (inflammation of the vagina)
🩺 Cervical polyps and/or ectropions

How should I seek help for bleeding in early pregnancy?

There are many causes of bleeding in early pregnancy and so it is essential that you see a healthcare professional for appropriate assessment, diagnosis and treatment (1-4).
If your bleeding is minimal and you are otherwise well, you can seek medical help in one of the following ways (1):
👩⚕️ From your GP or midwife (he/she might suggest you attend hospital depending on your symptoms).
👩⚕️ By contacting your local Early Pregnancy Assessment Unit, who may ask you to attend for an in-person appointment. If you are based in the UK, you can find your local Unit here.
👩⚕️ By phoning NHS 111 (available 24 hours a day, 7 days a week) if you feel that you need urgent medical assistance but it is not an emergency. NHS 111 can arrange an appointment for you with the appropriate healthcare team (e.g. in an Early Pregnancy Assessment Unit) depending on your clinical symptoms.
If you are bleeding heavily, have significant abdominal (tummy) pain, feel dizzy and/or faint and/or have any symptoms that you are imminently concerned about, you must seek urgent medical attention (1).
You can access urgent medical help by either (1):
👩⚕️ Attending your local Accident and Emergency department.
👩⚕️ Phoning your local emergency line (e.g. 999 in the UK).
❗Remember that if you have any symptoms of an ectopic pregnancy (see above)–particularly of a burst ectopic pregnancy–you must urgently get medical help from your local Accident and Emergency department or by phoning your local emergency line (10).
What will happen when I attend hospital for early pregnancy bleeding?
If you need to attend hospital for early pregnancy bleeding, it is likely that your healthcare professional will ask for information on: your clinical symptoms, previous pregnancies, current pregnancy, date of your last period and overall health (1).
Depending on your individual circumstance, you might need to have a combination of any of the following investigations (1):
👩⚕️ A urine pregnancy test.
👩⚕️ An ultrasound scan. Your doctor might suggest either a trans-abdominal ultrasound (where the scan probe is moved across your tummy) or a trans-vaginal ultrasound (where the scan probe is gently placed inside your vagina), or sometimes both. Neither a trans-vaginal or trans-abdominal ultrasound increases a woman’s likelihood of having a miscarriage.
👩⚕️ A speculum examination and/or examination of the vagina. This is done to check for pain and/or any clear cause for your bleeding.
👩⚕️ Blood tests (specifically to check your hCG hormone levels and blood group).
👩⚕️ Vaginal swabs for infection (e.g. STIs).
If you need to have an intimate examination or investigation, you should be offered a chaperone to accompany you throughout (1).
Outlook

Many women experience bleeding in early pregnancy and, although it can be an extremely distressing occurrence, it does not necessarily mean that there is a problem with your pregnancy. In fact, many women who have bleeding in the early stages of pregnancy will go on to give birth to happy, healthy babies (1-3).
However, early pregnancy bleeding can be a sign of more serious conditions, such as miscarriage or ectopic pregnancy (1-4, 10). Thus, it is essential that all women with bleeding in early pregnancy are assessed promptly by a healthcare professional, such as their maternity care team (1-4). If you have heavy bleeding, severe abdominal pain and/or any symptoms of a ruptured ectopic pregnancy (e.g. collapse), you must seek emergency medical assistance (1, 10).
It is important to remember that most women who receive more serious diagnoses (such as a molar pregnancy, ectopic pregnancy or miscarriage) are still able to have subsequent successful pregnancies (1,9,10).

References
(1) Bleeding and/or pain in early pregnancy. Royal College of Obstetricians and Gynaecologists. Published: September 2016. https://www.rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pregnancy/pi-bleeding-pain-early-pregnancy-mar20.pdf
(2) Vaginal bleeding in pregnancy. NHS. Published: January 2018. https://www.nhs.uk/conditions/pregnancy-and-baby/vaginal-bleeding-pregnant/
(3) Bleeding in pregnancy. Tommy’s. Published: October 2018. https://www.tommys.org/comment/9536
(4) Ectopic pregnancy: what else might cause pain or bleeding in early pregnancy? National Institute for Health and Care Excellence. Published: May 2018. https://cks.nice.org.uk/topics/ectopic-pregnancy/diagnosis/differential-diagnosis/
(5) Symptoms: miscarriage. NHS. Published: June 2018. https://www.nhs.uk/conditions/miscarriage/symptoms/
(6) Subchorionic hematoma and pregnancy risks: condition characterized by partial placental detachment. By: Krissi Danielsson. Medically reviewed by: Meredith Shur, MD. Very Well Family. Published: April 2020. https://www.verywellfamily.com/subchorionic-hematoma-2371262
(7) Perinatal outcomes in women with subchorionic hematoma: a systematic review and meta-analysis. Tuuli, Methodius G; Norman, Shayna M; Odibo, Anthony O, et al. Obstetrics & Gynecology. Volume: 117(5), pages 1205-1212. Published: May 2011. https://pubmed.ncbi.nlm.nih.gov/21508763/
(8) Information about placental abruption. Tommy’s. Published: September 2016. https://www.tommys.org/pregnancy-information/pregnancy-complications/information-about-placental-abruption
(9) Molar pregnancy–information and support. Tommy’s. Published: February 2020. https://www.tommys.org/pregnancy-information/pregnancy-complications/baby-loss/molar-pregnancy-information-and-support
(10) Ectopic Pregnancy. Royal College of Obstetricians and Gynaecologists. Published: November 2016. https://www.rcog.org.uk/globalassets/documents/patients/patient-information-leaflets/pregnancy/pi-ectopic-pregnancy-mar20.pdf