When my second child, Coby, became increasingly more distressed at around 3 weeks, I started to wonder if he could have reflux. Fast forward another 4 weeks of constant crying, arched back, pulling on and off the breast, significant vomiting until I decided to seek specialist advice.
Reflux is extremely common, and is, to some extent, normal. However when you are the parent trying to manage this on a daily basis it can be incredibly upsetting to see your baby in pain, and makes any semblance of normal life challenging as your baby will only feel comfortable rocking in your arms!

We found a number of things that helped to improve our situation, including; the use of a dummy (something I was very reluctant to try initially!), the sling and cutting dairy out of my diet (he is exclusively breastfed).
Now, at 13 weeks, Coby is much more settled during the day and is able to sleep well in the crib (which is elevated at the head end). There are still good days and bad days, but mostly we are hoping to have avoided the need for medication (although it is still an option should we need it).



I am grateful to Dr Harriet Holme (registered nutrition consultant and experienced paediatrician) for writing this blog post with me. You can also find her on Instagram as @Healthyeatingdr.
What is reflux?
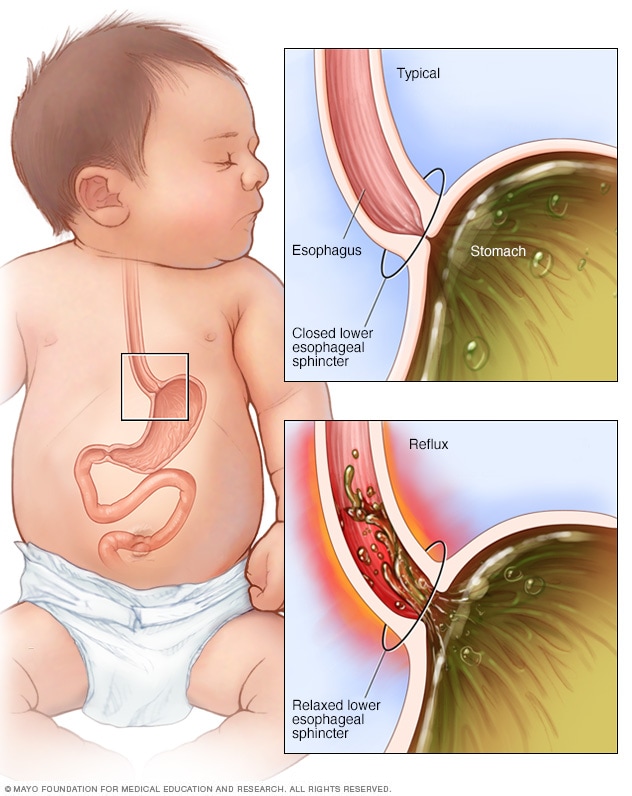
Reflux is regurgitation, mainly of liquid, back up the oesophagus/food pipe/gullet from the stomach.
There are two types of reflux, ‘physiological / functional’ and ‘non-physiological’. Up to 4 out of 10 babies will have reflux and 9 out of 10 of these will get better by themselves with time.
Physiological reflux
Most babies have a degree of physiological reflux, because they spend most of their time lying on their backs. They also have an under-developed muscle ring (sphincter) at the top of their stomach, which fails to prevent regurgitation.
This type of reflux is very common; the baby is well, putting on weight appropriately and will naturally improve by their first birthday, as the sphincter muscle develops and the baby becomes more upright.
Non-physiological reflux
This refers to reflux which is impacting on the health of the baby and is frequently called Gastro-Oesphageal Reflux Disease (GORD).
Recent evidence suggests that allergy, in particular to Cows’ Milk Protein, is the frequently the cause. Babies with this type of reflux may have a number of additional symptoms such as:
- Being difficult to settle
- Arching after feeds and drawing their legs up
- Explosive poos or constipation
- Blood in their poo
- Making rattling noises
- Poor weight gain
- Coughing or gagging during and after feeds
- Frequent vomiting after and between feeds
- Eczema before 6 months of age
- Cough
Since the regurgitated milk is also mixed with stomach acid, this can create discomfort for the baby. Some babies respond to this discomfort by being put off feeding (termed oral aversion), or want to feed all the time, in an attempt to keep down the acidic milk, and soothe their oesophagus/food pipe.
Most babies will vomit the regurgitated milk, but a minority do not, and this is termed ‘silent’ reflux. These babies often have milk in their mouth between feeds from regurgitation, even if they don’t vomit.
The most common allergy that underpins reflux is due to a reaction to a protein in cows’ milk called Cow’s Milk Protein Allergy (CMPA). Babies with CMPA need to be assessed by a qualified medical practitioner. If your baby has CMPA then all items with cows’ milk protein need to be avoided. For around 50% of babies there is also a soya intolerance so this should be avoided too.
There are a number of really simple positional changes that can help your baby with the symptoms of reflux:
- Elevate the head end of the cot (from the floor rather than placing something under the mattress)
- Avoid placing baby flat even for changing
- Hold baby upright after each feed for approximately 20 minutes
- Don’t bounce baby, as this is like ‘shaking a milk jug’, instead soothe by stroking, or swaying
- Try a dummy, which helps by drawing the milk down the oesophagus, because of the stimulation of sucking (non-nutritive sucking)
- If you are breastfeeding and have very fast let down, try a nipple shield or feed against gravity by lying on your back, to slow the flow down
When to see a doctor
- If you have concerns about your baby
- If the regurgitation becomes more forceful, and the vomit is expelled with such force that it lands some distance away.
- If your baby brings up milk that is green or yellowy green, or if it looks as though it has blood in it.
- If your baby has any new problems.
- If your baby is very distressed and you can’t soothe them.
- If you baby can’t feed.
- If you baby isn’t putting on weight.
What will the doctor do
Your doctor will take a history and find out more information about your baby, the vomiting, any additional symptoms and feeding.
In some cases, they might arrange for your baby to have some investigations if there is doubt about the diagnosis, or additional concerns.
What your doctor might prescribe
Previously when a baby was diagnosed with reflux they might have been treated first with anti-reflux medications. A few years ago, this changed and now first line treatment is to exclude an allergic cause.
This will mean an exclusion diet for the mother while breastfeeding for at least 4-8 weeks to determine if the symptoms improve.
In cases where there are still significant symptoms, your doctor might consider a trial of anti-acid medications such as a proton pump inhibitor like lansoprazole or omeprazole; however, there is limited evidence that these work in children under 1 year of age.
If your baby has been diagnosed with CMPA, have a look at my blog about Plant Based Milks and what to look out for when you are choosing one.
Colic
Colic is used as a catch all term for a baby who is unsettled between 6 weeks to 6 months old and they cry more than 3 hours a day, 3 days a week for at least 1 week.
If you are concerned your baby is irritable, or you are unable to soothe them, you should seek medical advice.
Colic and reflux often start at a similar time and can be confused, but a baby with colic has none of the symptoms associated with reflux, and the diagnosis should only be made if your baby is otherwise well.
There are some simple strategies you can try to soothe your baby with colic:
- Swaddle
- Rocking
- Cuddle them
- Winding them
- Giving them a warm bath
- White noise
There is very little evidence to support the use of anti-colic drops or manipulating the bones in your baby’s head (cranial osteopathy).
If your baby has been reviewed by a doctor and found to be otherwise well, you might find the purplecrying website useful.
More about Dr Harriet Holme
I studied medicine at the University of Cambridge, and have over a decade of experience in academic clinical practice as a paediatrician. Additionally I have a PhD in genetics, and use these uniquely developed scientific and clinical skills for the benefit of my private clients and students, exclusively consulting as a Registered Nutritionist (Associate of Nutrition) and lecturing in culinary science and nutrition.
Follow me @healthyeatingdr for more evidence based nutrition facts and see my website for more information about me and the services I offer www.healthyeatingdr.com
Check out my other post on ‘Eating well while breastfeeding’